|
|
Body knowledge in bytes: the health industry gears up for the 21st century
by
Paul Bentley
Article originally published in Online Currents August 2013 and reprinted with kind permission
of
Thomson Reuters.
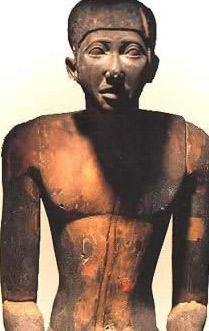 |
Imhoptep.
Image:
www.touregypt.net |
As you get older the thought that the years are running
out creates a compelling interest in health and medical
matters. Asking after the wellbeing of friends and
family becomes an extended part of any conversation. Too
many acquaintances disappear as their body parts give out.As you become more dependent on health and medical
services, you begin to search for more information in
the books on your shelf. The copy of an old St Johns
Ambulance First Aid Book, with drawings of men with
moustaches and broken arms in slings, and the medical
section of a forty-year old Pears Encyclopaedia
now no longer offer reliable answers.
Where do you go now for information on what’s wrong with
you? How is the health field responding to new ways of
doing things in the 21st century? How are
health industry developments affecting those who provide
dedicated service in this specialised field?
THE HEALTH FIELDWe have come a long way in learning how to deal with our
bodies. [i]
Medical practice is said to have begun with the Egyptian polymath, Imhoptep, who offered diagnoses and
treatments for 200 diseases in 2600 BC. His capabilities
as a doctor were no doubt reinforced by his other roles
as Chief Carpenter, Chief Sculptor, and Maker of Vases
in Chief. Two thousand years later, the Greek physician
Hippocrates introduced ethics by writing the Hippocratic
Oath.As civilisation emerged from the Middle Ages,
the medical profession continued to evolve. Women
began to play a more
influential role in the practice of medicine because of
the acuteness of their observation. Dr Mary Walker
changed views about senseless limb amputations during
the American Civil War. Florence Nightingale was
instrumental in reforming hospitals and the training of
nurses.
Some who set out to become doctors turned to other
professions because they couldn’t stomach some of the
things they needed to do. The French composer Hector
Berlioz, for example, on his first encounter at carving
up a dead body as a medical student, “leapt out of the
window and fled as though Death and all his hideous crew
were at [his] heels.” [ii]
After the
first painless surgery with general anaesthetic on a
live body was performed in 1846, new medical milestones
appeared at breathtaking speed.
Alexander Fleming discovered penicillin in 1928.
In 1967,
Christiaan Barnard successfully transplanted a human
heart. Louise
Brown, in 1978, became the first test tube baby. We have
already witnessed in quick succession during the 21st
century the development of robotic surgery, face
transplanting and human cloning. In
2013, the first baby in the United States was cured of
HIV. There is speculation that some visits to a doctor
will in future be a thing of the past because your
doctor will provide advice using Skype.
Today’s health and medical industry is a complex web of
forces.
According to the World Health Organisation (WHO),
countries spend more than US$4 trillion on health.[iii]
International health programs attempt to increase
longevity, eliminate inequities and persuade citizens to
look after themselves. The WHO’s
Millennium Development Goals aim to reduce child and
maternal mortality, improve nutrition, reduce mortality
due to HIV infection, tuberculosis and malaria, and
increase access to improved drinking water sources.[iv]
There are economic conundrums. Increased
spending on health by some countries has put pressure on
other national government programs. However, state and
local governments depend on national government support
to sustain local economies.
Cutting
health care costs is politically difficult.[v]
These pressures are evident in Australia, where
healthcare expenditure reached $134 billion in 2012. It
is increasing at twice the growth rate of GDP.[vi]
According to IBISWorld, the sector employs almost
780,000 people (6.8% of total employment). The growth in
the demand for services is a response to an ageing
population, lifestyle-related diseases, a free public
health system, growing household incomes and new
healthcare technologies.[vii]
About 70% of health expenditure is in the public sector.
There is a strong emphasis on primary care through
general practice, supported by Medicare.
The federal government’s attempt to implement healthcare
reforms is navigating the minefields of Australia’s
federated system and adversarial politics. In June 2013,
a series of articles in the Sydney Morning Herald
reported tensions between the public and private health
systems, the games being played between federal and
state governments, hospital budget pressures and
four-year waiting lists for elective surgery.
There is a medical underbelly. This year, the Global
Mail has been investigating the murky relation
between drug companies and doctors. It reports that, in
a worldwide pharmaceutical industry of $942 million,
pharmaceutical companies spend around $60 million a year
in Australia “educating” doctors. To work around the
bans on advertising prescription medications directly to
the public in Australia, the process of duchessing
doctors involves “ever-so-slight
culinary conflicts of interest”, free overseas trips,
lucrative consultancies and speaking gigs. Many doctors
admit to an obligation to return favours.
According to the medical journal
The Lancet
this is creating a “moral decay”. Patients may be given
drugs inappropriately. Expensive drugs are given
precedence over equally effective cheaper drugs. Without
access to transparent information, patients
do not know the extent of drug company influence.
Pharmaceutical promotional activities
push up health care costs. Efforts are underway to try
to limit the corrupting influence of pharmaceutical
payments on prescribing patterns.
Dr Ben Goldacre, a UK epidemiologist, says there is a
problem with the information architecture of
evidenced-based medicine. His book Bad Science
tackles misinformation about science in the media. A
companion polemic Bad Pharma examines the toxic
results of decades of hidden clinical trials. Although
governments wrestle with vested interests to tighten up
dodgy pharmaceutical marketing practices, the process
gets lost in the bureaucratic labyrinth. We have our
heads in the sand about fixing the problem.[viii]
HEALTH INFORMATION
As countries combat expanding costs, moving into the
electronic realm is not only unavoidable, it is an
imperative. People now have ready online access to
general information about health and medicine. But
managing the information on which the industry operates
will be a major test.
Online trends
The Pew Internet Project’s
reports about online health information set the scene.[ix]
Just over 80% of US adults now use the internet, 87% own
a mobile phone, and 45% own smartphones. A large number
of adults (70%) use doctors and other health care
professionals as their primary sources of information or
support. But 60% also got information or support from
friends and family.
Among internet users, 72% look online for health
information and 77% of these began their search using
Google, Bing, Yahoo or some other search engine. Another
13% started their search on a site specialising in
health information, such as WebMD. The most
commonly-researched topics are specific diseases or
conditions and treatments or procedures. Nearly 30% of
online health seekers said they had been asked to pay
for access to something they wanted to see online, but –
significantly - only 2% said they did so.
Seekers of online health information fall into a number
of categories.
- Adults with a chronic condition - 45% of US adults who
have at least one chronic condition such as high blood
pressure or diabetes.
- Adults with a disability - 27% of US adults live with a
disability; 42% of these look online for health
information.
- Older adults - 75% of adults are aged 65 years or older;
54% of adults in this age group use the internet; but
only 12% of this group own a smartphone. Around 30% of
adults in this age bracket look online for health
information.
- Caregivers -
39% of US adults
provide care for a loved one. 79% of caregivers have
access to the internet. Of those, 88% look online for
health information.
People turn to different
sources for different kinds of information. When they
have technical questions, professionals hold sway. When
a situation involves more personal issues – such as how
to cope or get quick relief -- non-professionals are
preferred. A small number of adults use technology to
track their health data, such as blood pressure, blood
sugar, headaches, or sleep patterns.
General reference sources
People now have ready access to general information
about health matters. As the Pew Internet Project
outlined, Google and other popular search engines will
be the first ports of call for most. Some will turn to government sites and other portals carrying the fingerprints of authority
such as Healthinsite (http://www.healthinsite.gov.au).
Some may have subscriptions to sites and mobile apps
like WebMD (http://www.webmd.com/)
and the Australian Mydoctor (http://www.mydr.com.au/).
Some will dig deeper by turning to the US National
Library of Medicine’s PubMed (http://www.ncbi.nlm.nih.gov/pubmed/)
and other digital resources. High
quality medical research and plain English summaries are
freely available from Wiley’s The Cochrane Library (http://www.thecochranelibrary.com/)
and its iPad app.
Your national, state, university or local library may
have the ALA Guide to Medical & Health Sciences Reference
and other printed sources and they will facilitate
access to online sources available from specialist
publishers and aggregators. For example, the
National Library of Australia’s e-resource collection of
freely available, licensed or onsite titles includes
Australasian Medical Index, Australian Institute
of Health and Welfare, Australian Medical
Pioneers Index, Australian Public Affairs
Information – Health, Australian Sport Database
Medical Subset, EBSCO’s Consumer Health Complete,
Drug Database, Encyclopedia of Australian
Science, Encyclopedia of Bioethics,
Encyclopedia of Science and Religion, Free
Medical Journals, Gale Encyclopedia of Science,
HealthInsite: Health Information for Australians,
Health and Society Database, Health Source
Nursing Academic Edition, Health and Wellness
Resource Gentre, HIV/AIDS Database,
Informit e-Library: Health, ISIHighlyCited.com,
MasterFILE Premier, Medlineplus Health
Information, Merck Manuals, PubMed Central,
and Rural and Remote Health Database.
Sector data and patient records
Managing industry data and patient records
electronically is widely seen as a solution for
responding to pressing needs. Better information will
help governments decide where to spend their money.
Better information may help improve productivity in a sector that attracts an
increasing proportion of public expenditure.
Solutions will involve the application of general
principles of information engineering and data
management on a grand scale and addressing major
impediments.
Since 2000, an increasing number of international
guidelines and performance indicators have guided high
level global action. In the United States, the recent
release of database-generated information on
charges in American hospitals revealed “an incoherent
system in which prices for critical medical services
vary seemingly at random -- from state to state, region
to region and hospital to hospital.” Some commentators
anticipate that making this information available is
unlikely to bring swift and radical change to pricing,
but they acknowledge that at least it is a good start.[x]
A report by the Sax Institute for the NSW Mental Health
Commission has found that more than $10 billion is being
poured annually into mental health treatment despite an
“information vacuum” about whether the treatments
represent value.[xi]
Improved productivity depends to some extent on
minimising errors. Most people you know will tell
stories not only about the skill and dedication of
health professionals, they will also complain about
medical misadventures. The Institute of Medicine claims
that 7,000 Americans die each year from preventable
paper prescription errors.[xii]
A few years ago the US Pharmacopeia MEDMARX database was found to have
176,409 medication error records, of which 25% involved
some aspect of computer technology as one of the causes
of the errors. A study in the Internal Medicine Journal showed that 10% of
patients at Maroondah Hospital in Melbourne left
hospital with the wrong diagnosis in their medical
records and half of patient records were missing
significant clinical information.[xiii]
According
to Sandra Boodman, the number of errors – through
misdiagnoses, medication errors and surgery on the wrong
patient or body parts – is high in America, but
addressing the issue is a challenge because it is
difficult for doctors to admit mistakes when their
reputations are at stake.[xiv]
Costs
are viewed as a major barrier to the widespread adoption
of e-health systems. Even after the initial expenditure
on implementation, there are ongoing maintenance and
training costs. Local GPs in particular may experience
difficulties in making the investment. Financial
incentives are needed. Despite evidence of cost savings
in some settings, doubts have been expressed about the
return on investment.
According to the New York Times, doctors and hospitals struggle to make
new records systems workwhile major vendors of systems reap enormous rewards.[xv]
Connecting medical records
involves sorting out complex privacy considerations.
There have been some legitimate fears and examples of
breaches of privacy and confidentiality.
Some doctors have expressed concerns that increased use of electronic health records
could expose them to an increased level of malpractice
litigation. The US Government Accountability Office
reported a few years ago that there is a "jumble of
studies and vague policy statements but no overall
strategy to ensure that privacy protections would be
built into computer networks linking insurers, doctors,
hospitals and other health care providers."[xvi]
Making health information available will involve
clarifying protocols for sharing data on a number of
levels, from complete openness to fully controlled
access.[xvii]
There have been suggestions that unintended adverse consequences have been caused by
system design deficiencies.
Improving the way the data is presented is seen as a
major challenge.
Health data standards, privacy laws, and the nature of
health systems complicate the design process. In an
effort to combat this problem, the US Department of
Veterans Affairs recently embarked on a Health Design
Challenge (http://healthdesignchallenge.com)
to assist in building open source design solutions for
patient electronic records across the country.
Suggestions are now being incorporated in Veterans
Affairs hospital systems.[xviii]
The need for better information engineering comes at a
time when the field of health informatics is in the
formative stages of its development. As a discipline
that embraces information management, knowledge
management, project management, ICT, clinical
informatics, health records and other topics, the
adoption of standards will be at the centre of its
deliberations. Yet, according
to John Kuranz and Barbara Gilles, purveyors of health
systems “manoeuvre to occupy or invent the standards
high ground and to capture the attention of the
marketplace, but they often bring ambiguity to the
discussion of process and confusion to the debate over
performance.” They cite the International Statistical
Classification of Diseases and Related Health Problems
and the American Medical Association’s Current
Medical Terminology among other language systems
heavily used, but further work, they say, is needed.[xix]
IT
Applications in Healthcare Technology
(ICS 35.240.80 IT) is one of a number of standards
covering health informatics. Standards Australia has
technical committees
working locally on the issue.
Creating sector-wide commitment to government-led
e-health systems is perhaps the major challenge. Glen Tullman, writing on the situation in the United States,
says the process of getting doctors to move into the electronic realm has
been
arduous and there isn’t conclusive evidence
that the use of electronic health records improves
patient care quality. Quoting a report from President’s
Council of Advisors on Science and Technology, he says
the impact of IT on health care over the past decade has
so far been modest. More physicians need to become part
of the system. The records need to be connected to each
other. And the systems that have already been installed
need to work better before it will help doctors,
patients and others improve health.[xx]
In Australia, a national e-health strategy, involving
the development of a shared electronic health records
system to address existing fragmentation, duplicate
effort and data inconsistencies, is being rolled out.
But the project is currently suffering from challenges
around the level of computerisation,
interoperability and the skills needed to make it work.[xxi]
The National E-Health Transition Authority
(http://www.nehta.gov.au/) has been established to lead
the uptake of e-health solutions and accelerate their
adoption. Health Direct Australia (http://www.healthdirect.org.au/)
has been set up to manage telephone health services, health information
websites and clinical governance structures to
streamline patient enquiries.
The Centre for Health
Record Linkage (http://www.cherel.org.au/)
is indicative of efforts underway to assist in
connecting researchers and policy makers to linked
health data. The National Broadband Network and other
technologies have the potential to revolutionise the
health sector.LIBRARY, ARCHIVAL AND MUSEUM SERVICES
Libraries, archives and museums have in the past been
good places for finding out what makes you tick. For
more than two centuries they have rendered valuable
services to the medical profession and the public at
large. In the age of ubiquitous computing, how are their
services being affected by online imperatives?
International libraries, archives and
museums
The largest biomedical library in the world is the
National Library of Medicine in the United States (NLM,
https://www.nlm.nih.gov). It traces its origins back
to 1818, when Dr Joseph Lovell, the first Surgeon
General of the Army, began building a reference
collection in his office. The library flowered in the
second half of the 19th century under John
Shaw Billings, a surgeon who transformed himself into a
librarian.
The library now has numerous databases, including
Medline, which is freely available on the Internet and searchable via
PubMed (http://www.ncbi.nlm.nih.gov/pubmed/),
other information, images and tutorials.
The NLM works with the National Network of Libraries of Medicine
to provide regional support throughout the United
States. During the early 1990s, it provided funding for the Manual for Cataloguing
Historical Medical Artifacts Using OCLC and the MARC
Format, prepared by the Ohio Network of Medical
History Collections. It hosts the
History of Medicine Finding Aids Consortium
http://www.nlm.nih.gov/hmd/consortium/index.html, a
union catalogue of primary source materials found in
special collections and archives throughout the country.
Other major medical libraries and archives in the United
States, include the Countway Library of Medicine (https://www.countway.harvard.edu)
at Harvard University and the Medical History Library at
Yale University (http://library.medicine.yale.edu/).
The US National Museum of Health and Medicine (http://www.medicalmuseum.mil/)
was founded as the Army Medical Museum in 1862 during
the Civil War and has achieved accolades for its
research on
infectious diseases and other health problems. Its
library and cataloguing system formed the basis for the
National Library of Medicine and its collection
today consists of about 25 million artefacts, including
skeletal specimens, preserved organs, medical equipment,
and historic medical documents. Other notable museums
include the Mütter Museum at the
College of Physicians (http://www.collegeofphysicians.org/mutter-museum/)
and the Dittrick Museum at Case Western Reserve
University in Cleveland, Ohio (http://www.case.edu/artsci/dittrick/museum/).
The largest medical library in Europe is the German
National Library of Medicine
(http://www.zbmed.de/en/home.html), which operates as
the official European agent for the US National Library
of Medicine.
One of the oldest medical collections in Europe can be
found at the Museum of History of Medicine at the
University Rene Descartes, Paris.[xxii]
It opened in 1954 but traces its origins back to 1769,
when two rooms were devoted to “ancient collections” at
the Academy and College of Surgery.
A new book on medical museumsexplores the collections of 15 leading museums
in Europe and the United States.[xxiii]
And a list of London health and medical museums and
archives can be found at
http://www.medicalmuseums.org/.
Recent exhibitions in London have drawn attention to the
value of museums as places of education and research.
The popularity of the exhibition, Death: A Self-Portrait, presented by the Welcome Collection
(www.wellcomecollection.org)
stimulated plans for a £17 million expansion. At the Museum of
London Archaeology, the exhibition Doctors, Dissection and Resurrection Men http://www.museumoflondonarchaeology.org.uk/)
explored scientific endeavours in the search for
knowledge about anatomy in the 19th century
and lifted the lid on the associated shadowy trade of
bodysnatching. Old bodies excited the public imagination
when the bones of Richard III were dug up from a
Leicester council car park and the British Museum
presented one of its oldest mummies, the Gebelein Man,
on a digital autopsy table.
The interests of libraries, archives and museums are
served by a large number of professional associations
and networks. Prominent among these is the Medical
Library Association (http://www.mlanet.org/), with
more than 4,000 members and partners worldwide. Other
groups of librarians include the Biomedical and Life Science Division and Pharmaceutical
and Health Technology Division of the Special Libraries
Association (http://www.sla.org/), Archivists and Libraries in the History of Health
Sciences (http://www.alhhs.org),
the Science, Technology and Health Care Roundtable of
the Society of American Archivists
(http://www.archivists.org/saagroups/sthc/index.html),
and the Canadian Health Libraries Association (http://www.chla-absc.ca/).
Among European bodies are the Health Libraries Group of
the Chartered Institute of Libraries and Information
Professionals,[xxiv]
a library group associated with the National Health
Service in the England (http://www.libraryservices.nhs.uk/),
the German Association for Medical Librarianship (AGMB) (http://www.agmb.de/)
and the Medical Museums Association
http://www.cwru.edu/affil/MeMA/memahome.htm)
International bodies include the International
Federation of Library Associations’ Health and
Biosciences Libraries Section (http://www.ifla.org/health-and-biosciences-libraries),
the European Association for Health Information and
Libraries (http://www.eahil.net/),
and the European Association of Museums of the History
of Medical Sciences (http://www.aemhsm.net/).Allied health and medical information groups overseas
include the International Medical Informatics Association
(http://www.imia-medinfo.org/new2/),
the Healthcare Information and Management Systems Society
(http://www.himss.org/), the American Society of Health
Informatics Managers (http://www.ashim.org/),
and the American Health Information Management
Association (http://www.ahima.org/).
Australian libraries, archives and
museums
Professional bodies in Australia have recently explored
issues facing their members.
Health Libraries Inc (http://www.hlinc.org.au/), in
partnership with the Australian Library and Information
Association, has published Questions of Life and
Death, a report on the value of health library and
information services in Australia. It reports that,
despite a significant increase in users and high levels
of satisfaction in services, the budgets of services,
their staffing levels and floor areas have declined.
Reductions in staff hours have had a detrimental effect
on services. There is uncertainty about the future.[xxv]
ALIA’s own group, Health Libraries Australia
(http://www.alia.org.au/groups/HLA),
has published
Health
Librarianship Workforce and Education: Research to Plan
the Future,
drawing on similar reports on the changing circumstances of health
librarians overseas, to describe the situation here. The
expectations and habits of consumers of health
information have changed. Traditional library work is
diminishing. Professional boundaries are blurring.
Emerging areas of work are being claimed by other
professional groups.[xxvi]
Health Libraries Australia is developing a framework of
competency-based standards in the quest for continued
credibility.
Allied professional groups include the Chief Health
Librarians Forum Australia (http://www.fhhs.health.wa.gov.au/inforx/aboutus.html),
Health Informatics Society of Australia (http://www.hisa.org.au/),
Health Information Management Association of Australia (http://www.himaa2.org.au/),
Australian and New Zealand Society of the History of
Medicine (http://www.anzshm.org.au/),
the
Asia Pacific Association for Medical Informatics (http://www.apami.org/),
and the
Australasian College of Health Informatics
(http://www.achi.org.au/). It has proved difficult to
sustain a viable professional association in the museum
sector after the Health and Medicine Museums group
within Museums Australia folded up in 2006.
Health Libraries
Australia, based on listings in the Australian Libraries
Gateway, has estimated that there are 427 health and
medical libraries in Australia. They include facilities
in hospitals, universities, research institutes,
pharmaceutical companies, government departments,
regional health services, professional colleges,
not-for-profit and community organisations, and parts of
public library services. The Guide to Health and
Medicine Collections, Museums and Archives in Australia,
published by Museum Australia’s Health and Medicine
Museums division in 1999, listed 185 specialist
collections and more than 200 other collections with
health and medical material.
Australian health and medical museums were recently
explored in Museums Australia Magazine.[xxvii]
Their rich variety are exemplified in the Medical
Heritage Trail at the University of Sydney, where 19
museums, buildings, libraries, monuments and artworks
are located on campus, including the Pathology Museum’s
Interactive Centre for Human Diseases (http://sydney.edu.au/medicine/pathology/museum/).
At Museums Australia’s national conference in May 2013,
Jacqueline Healy outlined exciting building plans and
collection management strategies that tie together
a number of notable collections managed by the
University of Melbourne (http://museum.medicine.unimelb.edu.au/).
Museum, library and archival services in hospitals
include the Royal Prince Alfred Hospital (http://www.sswahs.nsw.gov.au/rpa/museum)
and Sydney Hospital, the oldest in Australia, where the
Lucy Osborn-Nightingale Museum, operating with
volunteers, has a morbid anatomy collection and
historical material.
Collections and services that have been developed by
professional bodies include the Harry Daley Museum and
the Richard Bailey Library of the Australian Society of
Anaesthetists in Edgecliff, Sydney
(http://www.asa.org.au), and its counterpart in
Melbourne, the Geoffrey Kaye Museum of Anaesthetic
History at the Australian and New Zealand College of
Anaesthetics (http://www.anzca.edu.au/ ). The Royal
Australian College of Physicians’ History of
Medicine Library, with approximately 40,000 items and a
collection of antique medical instruments (http://www.racp.edu.au/page/library),
is promoted as Australia's most significant collection
of medical history.
Substantial collections of diverse material are also
found in national and state institutions, For example,
Museum Victoria (http://museumvictoria.com.au/) has
general medical and surgical equipment used by Sir
Edward "Weary" Dunlop, research equipment and medicinal
samples from the Commonwealth Serum Laboratories,
1918-1984, and other formed collections of Melbourne
medical and dental practices. The National Museum of Australia (http://www/nma.gov.au)
has Fred Hollows’ personal collection and objects from his trachoma program, as well as
Australian Institute of Anatomy collections,
comprising Aboriginal human ancestral remains
once housed in the building that is now home to the
National Film and Sound Archives. Asylum patient records
and other documentation are held by State Records NSW.[xxviii]
Pulling data together to make the richness of these
collections more accessible has some way to travel.
Research Data Australia (RDA,
http://researchdata.ands.org.au/) lists nearly 800 data
sets and collections in the area of health and medical
science. Trove (http://trove.nla.gov.au/),
already populated with relevant information from RDA,
libraries and commercial databases, is keen to improve
its coverage and welcomes discussions about exposing
specialist collections to the national discovery
service.
As reported in Online Currents in 2012, the
National Broadband Network has led to regional digital
hubs that offer potential for new relationships between
local libraries and health services.[xxix]
THE DIAGNOSIS
Medicine is a speculative art that relies on scientific
information. Good health and the mitigation of diseases
are in the hands of patients as well as doctors. Some
doctors think patients are an
essential member of the clinical care team.[xxx]
The decision by Hollywood star Angelina Jolie
illustrates the point. In deciding to have a double
mastectomy to minimise the risk of future cancer evident
in her family history, she underscored the need for
clear information, good communication, shared
responsibility and a dose of courage.
Governments around the world have initiated e-health
strategies to help doctors to diagnose ailments and give
patients a better understanding of what’s going on with
their bodies. There have been teething problems in
implementing e-health systems and there are barriers
that need to be overcome to sort out underlying
problems.
Those working in libraries, archives and museums in the
health and medical field, like their colleagues in other
fields, face ongoing challenges. Myriad professional
groups search for greater unity of purpose. In a world
where the services of intermediaries are being reshaped,
there are fresh opportunities for those involved in
constructing systems and services that lead governments,
doctors and patients to online resources.
Endnotes
Bronia Renison, Director
Library Services, Townsville Health Library,
provided a number of useful suggestions on sources
and style.
[ii]
Fitzharris L, “Mangling the Dead: Dissection,
Past and Present,” The Lancet, 12 January 2012.
[xi]
Corderoy A, “Assessment of Mental Heath
Treatment Hurt by Lack of Data”, Sydney Morning
Herald, 13 June 2013
[xxiii]
Medical Museums: Past, Present, Future; edited
by S J M M Alberti and E Hallam, The Royal
College of Surgeons of England, 2013
[xxvii]
Bentley P, “Australia’s First Hospital and the
Landscape of Health and Medical Museums Today.”
(2012) vol 21 no 2 Museums Australia Magazine:
34-36
[xxix]
Bentley P, “Reinventing Libraries for the Mobile
Flaneurs: The Odyssey Continues” (2012) 26 OLC
295
[xxx]
Gray, JAM. The
Resourceful Patient (eRosetta Press, Oxford
2002
Non-commercial viewing,
copying, printing and/or distribution or reproduction of
this article or any copy or material portion of the
article is permitted on condition that any copy of
material portion thereof must contain copyright notice
referring "Copyright ©2013 Lawbook Co t/a Thomson Legal
& Regulatory Limited." Any commercial use of the article
or any copy or material portion of the article is
strictly prohibited. For commercial use, permission can
be obtained from Lawbook Co, Thomson Legal & Regulatory
Limited, PO Box 3502, Rozelle NSW 2039,
www.thomson.com.au
p
|